Other General Surgical Procedures
Dr. Vamsi, General Surgeon, Bangalore | Patient Education | Other General Surgeries
1. Haemorrhoids / Piles Surgery
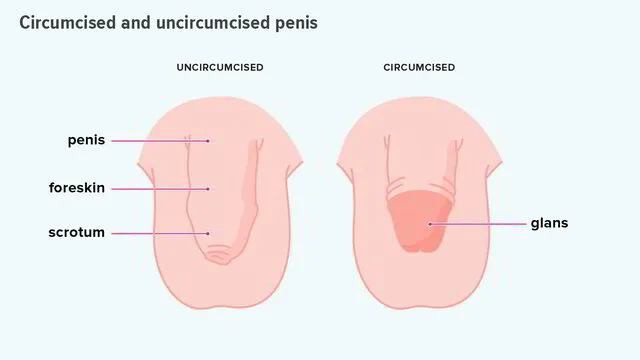
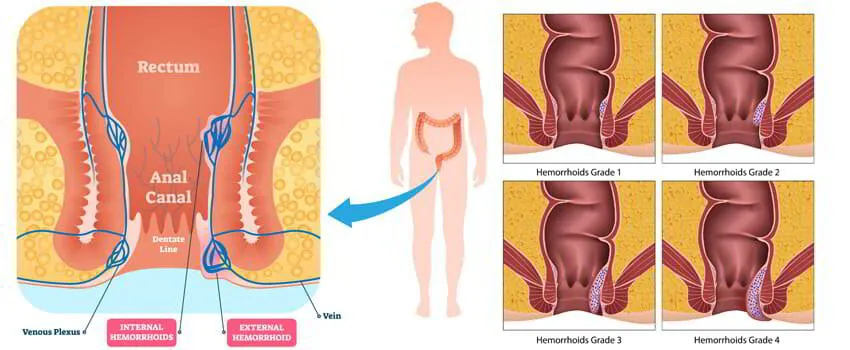
Haemorrhoids are swollen/enlarged veins in the lowest part of your rectum and anus. Haemorrhoids are one of the most common causes of rectal bleeding. Haemorrhoids can either be internal or external. Internal haemorrhoids develop within the anus or rectum. External haemorrhoids develop outside of the anus.
Symptoms of haemorrhoids include painless bleeding per rectum, pain and itching around the anus, faecal leakage and painful bowel movements. If blood pools in an external haemorrhoid and forms a clot (thrombus), it can result in thrombosed haemorrhoids which causes severe pain where emergency surgical intervention is needed.
Treatment ranges from simple diet modification and laxatives to surgeries depending upon the stage at which patient presentation. Surgery may be open hemorrhoidectomy, which is more traditional or stapler hemorrhoidectomy, which is more popular due to advantages like less pain and discomfort.
2. Fissure in Ano
An anal fissure (fissure-in-ano) is a small tear in the mucosa that lines the opening of the anus. Fissures typically cause severe pain and bleeding with bowel movements. Fissures are quite common in the general population, but are often confused with other causes of pain and bleeding, such as haemorrhoids/piles.
The typical symptoms of an anal fissure include pain and bleeding with bowel movements, most often when you pass hard stools. Patients experience severe pain during, and especially after a bowel movement, lasting from several minutes to a few hours. Patients often notice bright red blood from the anus that can be seen on the toilet paper or on the stool. Between bowel movements, patients with anal fissures are often relatively symptom-free.
Acute fissure may be managed medically whereas chronic fissure may require surgical intervention in the form of controlled division of the part of the internal anal sphincter muscle (sphincterotomy). The success rates reported to be over 90%.
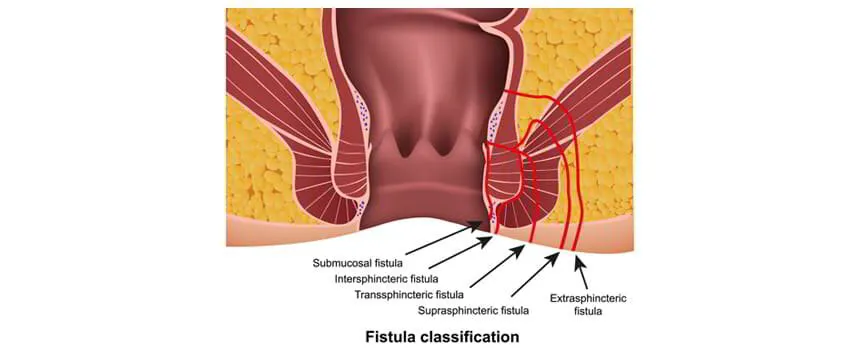
3. Fistula in Ano
An anal fistula is an infected tunnel between the skin and the anus, the muscular opening at the end of the digestive tract. Most anal fistulas are the result of an infection in an anal gland that spreads to the skin. It usually follows an infection that didn’t heal the right way.
Majority of the times fistula is caused by an abscess. It’s rare, but they can also come from conditions like tuberculosis, sexually transmitted diseases, or an ongoing illness that affects your bowels, such as Crohn’s disease or ulcerative colitis.
Symptoms include pain, redness, fever, swelling and discharge of blood or pus from a hole near your anus. Surgery is usually required to treat anal fistula. There are two types of surgeries available. One is a traditional open method, where the muscles around fistula cut and fistula laid open. Other is laser method, which is increasingly popular nowadays because of advantages like no cuts or no stitches, less pain and early return to normal activity.
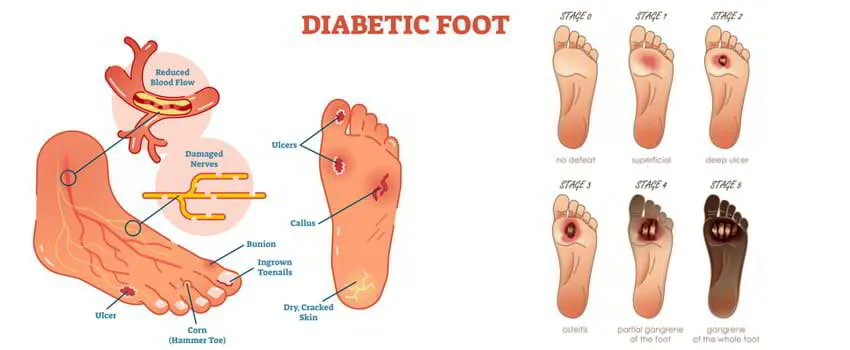
4. Diabetic foot ulcer
Foot ulcers are most commonly occur as a complication of poorly controlled diabetes, forming as a result of skin tissue breaking down and exposing the layers underneath. They’re most common under your big toes and the balls of your feet, and they can affect your feet down to the bones.
Ulcers form due to a combination of various factors like lack of feeling in the foot, poor circulation, foot deformities, irritation (such as friction or pressure), and trauma. The duration of diabetes also plays an important risk factor. Patients who have diabetes for many years can develop neuropathy, a reduced or complete lack of ability to feel pain in the feet due to nerve damage caused by increased blood glucose levels over time. The nerve damage often can occur without pain, and one may not even be aware of the problem.
All people with diabetes can develop foot ulcers and foot pain at one point in their lifetime, but good foot care can help prevent them. Treatment for diabetic foot ulcers and foot pain varies depending on their causes. It ranges from simple glycemic control to amputation in severe cases. In majority of patients appropriate treatment of a diabetic foot ulcer include prevention of infection, taking the pressure off the area, called “off-loading” footwear, managing blood glucose level and surgical debridement depending on the presentation.
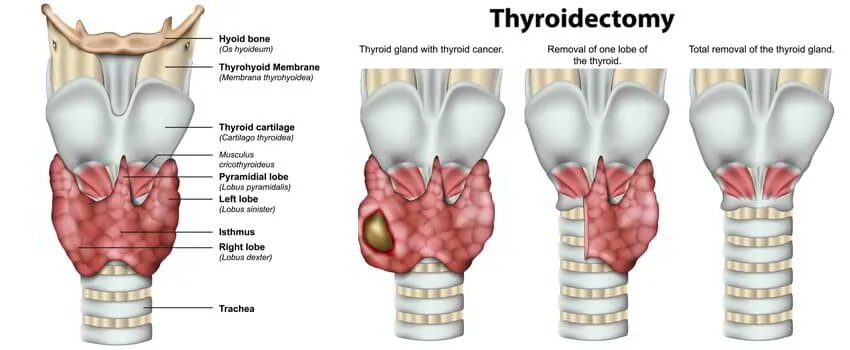
5. Thyroidectomy / Thyroid Surgery
A thyroidectomy is an operation that involves the surgical removal of all or part of the thyroid gland. General, endocrine or head and neck surgeons often perform a thyroidectomy when a patient has thyroid cancer or some other condition of the thyroid gland or goiter.
A thyroidectomy is traditionally a minimally invasive surgery performed through a small horizontal incision in the front of the neck. The entire thyroid gland may be removed or just a single lobe, a portion of a lobe and the isthmus or other structures. Depending on the extent of the operation, patients may need to take the drug levothyroxine, an oral synthetic thyroid hormone.
6. Excision of lumps
Excision of lumps and bumps refers to any minor procedure for skin or subdermal lesions, such as warts, moles, cysts or lipomas. These are typically undertaken under local anaesthesia in a day surgery unit.
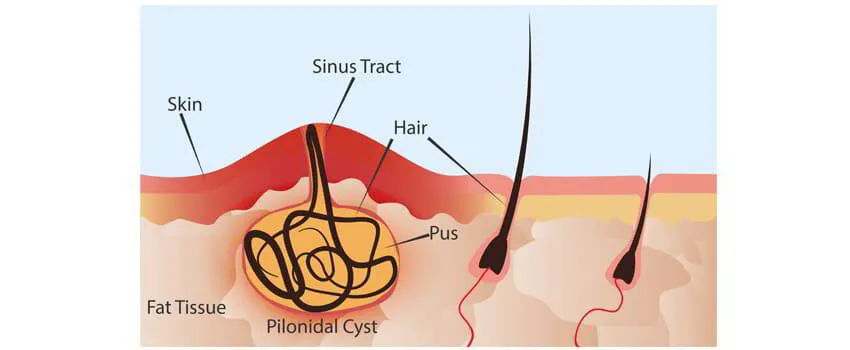
7. Pilonidal Sinus and Abscess
A pilonidal sinus (PNS) is a small hole or tunnel in the skin. It may fill with fluid or pus, causing the formation of a cyst or abscess. It occurs in the cleft at the top of the buttocks. A pilonidal cyst usually contains hair, dirt, and debris. It can cause severe pain and can often become infected. If it becomes infected, it may ooze pus and blood and have a foul odor.
A PNS is a condition that mostly affects men and is also common in young adults. It’s also more common in people who sit a lot, like cab drivers.
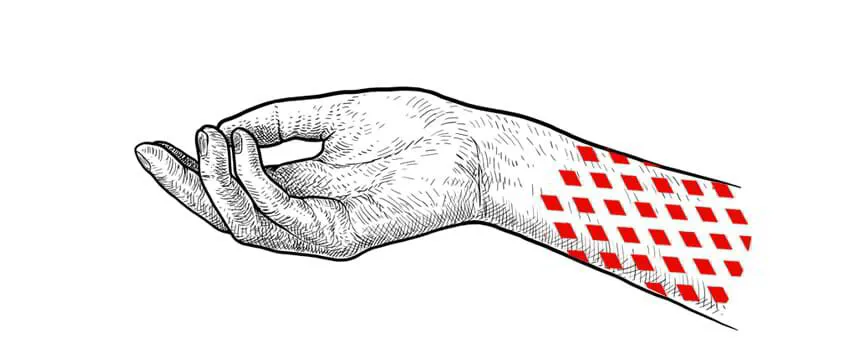
8. Skin Grafting
Skin grafting is a surgical procedure that involves removing skin from one area of the body and moving it, or transplanting it, to a different area of the body. This surgery may be done if a part of your body has lost its protective covering of skin due to burns, injury, or illness.
A PNS is a condition that mostly affects men and is also common in young adults. It’s also more common in people who sit a lot, like cab drivers.
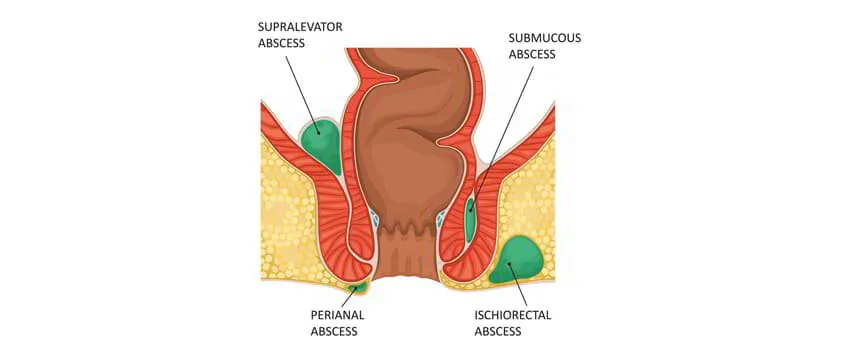
9. Incision and Drainage for Abscess
An abscess is a confined collection of pus surrounded by inflamed tissue. Most abscesses are found on the extremities, buttocks, breast, axilla, groin, and areas prone to friction or minor trauma, but they may be found in any area of the body. Abscesses are formed when the skin is invaded by microorganisms. Cellulitis may precede or occur in conjunction with an abscess. The two most common microorganisms leading to abscess formation are Staphylococcus and Streptococcus.
Treatment of an abscess is primarily through incision and drainage (I&D;). Smaller abscesses (5 mm) may resolve spontaneously with the application of warm compresses and antibiotic therapy. Larger abscesses will require I&D; as a result of an increase in collection of pus, inflammation, and formation of the abscess cavity, which lessens the success of conservative measures.
10. Wound Debridement
Debridement is the removal of dead (necrotic) or infected skin tissue to help a wound heal. It's also done to remove foreign material from tissue. The procedure is essential for wounds that aren't getting better. Usually, these wounds are trapped in the first stage of healing. When bad tissue is removed, the wound can restart the healing process.
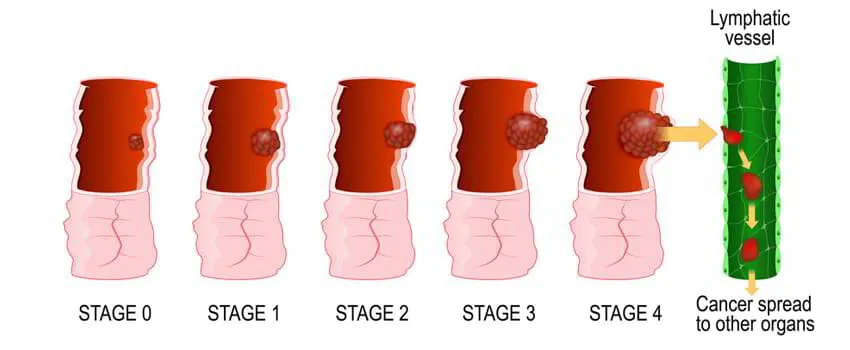
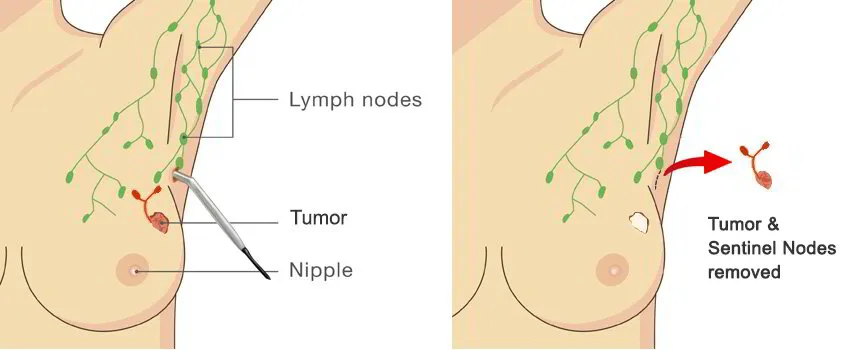
11. Lymph node Biopsy
Lymph node biopsy is a test in which a lymph node or a piece of a lymph node is removed for examination under a microscope. The lymphatic system is made up of several lymph nodes connected by lymph vessels. The nodes produce white blood cells that fight infections.
12. Varicose Veins Surgery
Surgery. If endothermal ablation treatments and sclerotherapy are unsuitable for you, you'll usually be offered a surgical procedure called ligation and stripping to remove the affected veins. Varicose vein surgery is usually carried out under general anaesthetic, which means you will be asleep during the procedure.
13. Limb Amputation
Amputation is the removal of a limb by trauma, medical illness, or surgery. As a surgical measure, it is used to control pain or a disease process in the affected limb, such as malignancy or gangrene. In some cases, it is carried out on individuals as a preventive surgery for such problems.
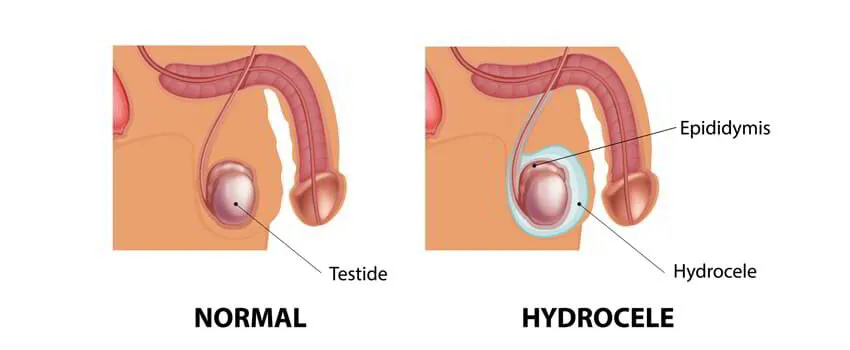
14. Surgery for Hydrocele
A hydrocele is a swelling in the scrotum, the thin sac that holds the testicles. It happens when too much fluid builds up inside. The condition is most common in newborns, though it can happen to anyone with a scrotum.
It may sound or look serious, even painful, but it won’t hurt your baby. It might go away on its own, though you should still see the doctor about it.
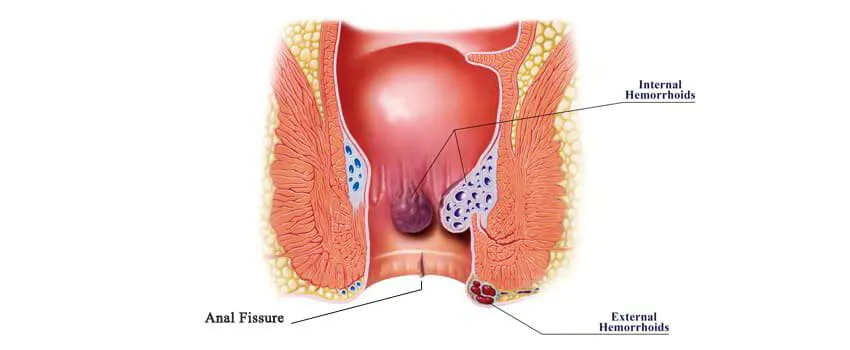
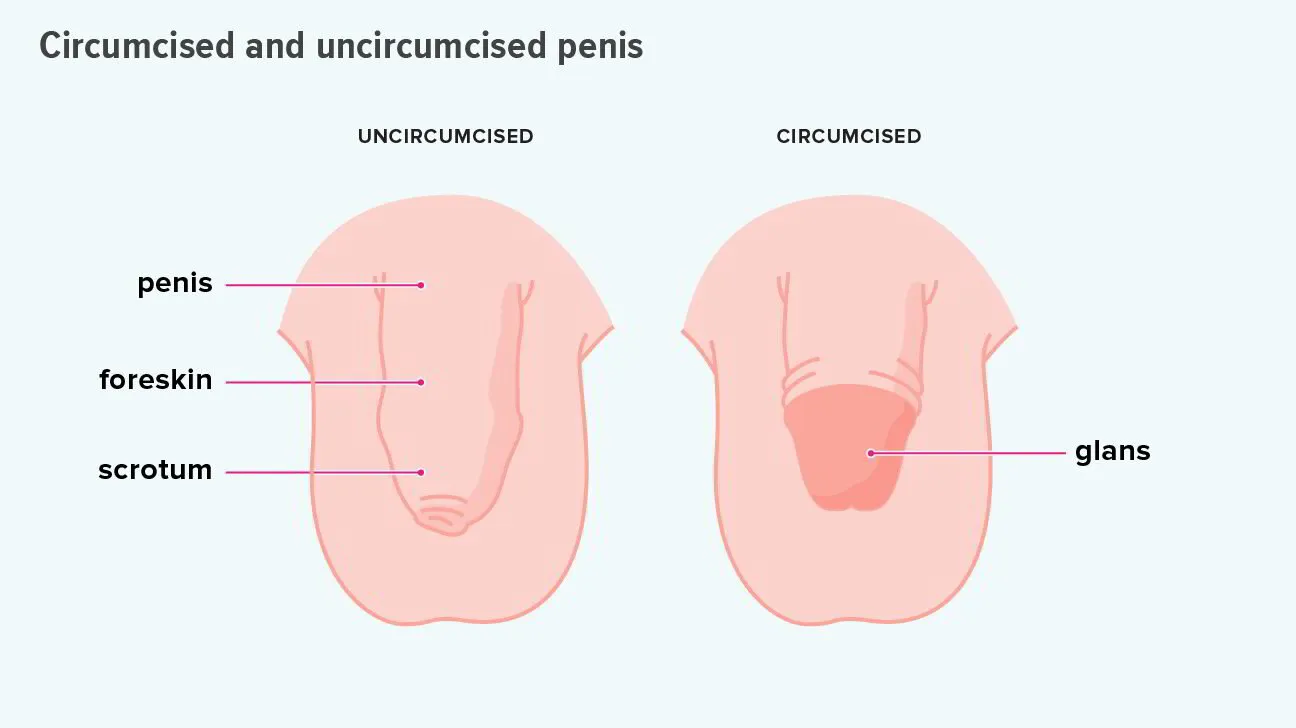
15. Circumcision
Circumcision is the removal of the foreskin from the human penis. In the most common procedure, the foreskin is opened, adhesions are removed, and the foreskin is separated from the glans. After that, a circumcision device may be placed, and then the foreskin is cut off
| Page Contents
- Haemorrhoids / Piles Surgery
- Fissure in Ano
- Fistula in Ano
- Diabetic foot ulcer
- Thyroidectomy / Thyroid Surgery
- Excision of lumps
- Pilonidal Sinus and Abscess
- Skin Grafting
- Incision and Drainage for Abscess
- Wound Debridement
- Lymph node Biopsy
- Varicose Veins Surgery
- Limb Amputation
- Surgery for Hydrocele
- Circumcision
____________________
____________________
____________________
____________________
1. Haemorrhoids / Piles Surgery
Haemorrhoids are swollen/enlarged veins in the lowest part of your rectum and anus. Haemorrhoids are one of the most common causes of rectal bleeding. Haemorrhoids can either be internal or external. Internal haemorrhoids develop within the anus or rectum. External haemorrhoids develop outside of the anus.
Symptoms of haemorrhoids include painless bleeding per rectum, pain and itching around the anus, faecal leakage and painful bowel movements. If blood pools in an external haemorrhoid and forms a clot (thrombus), it can result in thrombosed haemorrhoids which causes severe pain where emergency surgical intervention is needed.
Treatment ranges from simple diet modification and laxatives to surgeries depending upon the stage at which patient presentation. Surgery may be open hemorrhoidectomy, which is more traditional or stapler hemorrhoidectomy, which is more popular due to advantages like less pain and discomfort.
2. Fissure in Ano
An anal fissure (fissure-in-ano) is a small tear in the mucosa that lines the opening of the anus. Fissures typically cause severe pain and bleeding with bowel movements. Fissures are quite common in the general population, but are often confused with other causes of pain and bleeding, such as haemorrhoids/piles.
The typical symptoms of an anal fissure include pain and bleeding with bowel movements, most often when you pass hard stools. Patients experience severe pain during, and especially after a bowel movement, lasting from several minutes to a few hours. Patients often notice bright red blood from the anus that can be seen on the toilet paper or on the stool. Between bowel movements, patients with anal fissures are often relatively symptom-free.
Acute fissure may be managed medically whereas chronic fissure may require surgical intervention in the form of controlled division of the part of the internal anal sphincter muscle (sphincterotomy). The success rates reported to be over 90%.
3. Fistula in Ano
An anal fistula is an infected tunnel between the skin and the anus, the muscular opening at the end of the digestive tract. Most anal fistulas are the result of an infection in an anal gland that spreads to the skin. It usually follows an infection that didn’t heal the right way.
Majority of the times fistula is caused by an abscess. It’s rare, but they can also come from conditions like tuberculosis, sexually transmitted diseases, or an ongoing illness that affects your bowels, such as Crohn’s disease or ulcerative colitis.
Symptoms include pain, redness, fever, swelling and discharge of blood or pus from a hole near your anus. Surgery is usually required to treat anal fistula. There are two types of surgeries available. One is a traditional open method, where the muscles around fistula cut and fistula laid open. Other is laser method, which is increasingly popular nowadays because of advantages like no cuts or no stitches, less pain and early return to normal activity.
4. Diabetic foot ulcer
Foot ulcers are most commonly occur as a complication of poorly controlled diabetes, forming as a result of skin tissue breaking down and exposing the layers underneath. They’re most common under your big toes and the balls of your feet, and they can affect your feet down to the bones.
Ulcers form due to a combination of various factors like lack of feeling in the foot, poor circulation, foot deformities, irritation (such as friction or pressure), and trauma. The duration of diabetes also plays an important risk factor. Patients who have diabetes for many years can develop neuropathy, a reduced or complete lack of ability to feel pain in the feet due to nerve damage caused by increased blood glucose levels over time. The nerve damage often can occur without pain, and one may not even be aware of the problem.
All people with diabetes can develop foot ulcers and foot pain at one point in their lifetime, but good foot care can help prevent them. Treatment for diabetic foot ulcers and foot pain varies depending on their causes. It ranges from simple glycemic control to amputation in severe cases. In majority of patients appropriate treatment of a diabetic foot ulcer include prevention of infection, taking the pressure off the area, called “off-loading” footwear, managing blood glucose level and surgical debridement depending on the presentation.
5. Thyroidectomy / Thyroid Surgery
A thyroidectomy is an operation that involves the surgical removal of all or part of the thyroid gland. General, endocrine or head and neck surgeons often perform a thyroidectomy when a patient has thyroid cancer or some other condition of the thyroid gland or goiter.
A thyroidectomy is traditionally a minimally invasive surgery performed through a small horizontal incision in the front of the neck. The entire thyroid gland may be removed or just a single lobe, a portion of a lobe and the isthmus or other structures. Depending on the extent of the operation, patients may need to take the drug levothyroxine, an oral synthetic thyroid hormone.
6. Excision of lumps
Excision of lumps and bumps refers to any minor procedure for skin or subdermal lesions, such as warts, moles, cysts or lipomas. These are typically undertaken under local anaesthesia in a day surgery unit.
7. Pilonidal Sinus and Abscess
A pilonidal sinus (PNS) is a small hole or tunnel in the skin. It may fill with fluid or pus, causing the formation of a cyst or abscess. It occurs in the cleft at the top of the buttocks. A pilonidal cyst usually contains hair, dirt, and debris. It can cause severe pain and can often become infected. If it becomes infected, it may ooze pus and blood and have a foul odor.
A PNS is a condition that mostly affects men and is also common in young adults. It’s also more common in people who sit a lot, like cab drivers.
8. Skin Grafting
Skin grafting is a surgical procedure that involves removing skin from one area of the body and moving it, or transplanting it, to a different area of the body. This surgery may be done if a part of your body has lost its protective covering of skin due to burns, injury, or illness.
A PNS is a condition that mostly affects men and is also common in young adults. It’s also more common in people who sit a lot, like cab drivers.
9. Incision and Drainage for Abscess
An abscess is a confined collection of pus surrounded by inflamed tissue. Most abscesses are found on the extremities, buttocks, breast, axilla, groin, and areas prone to friction or minor trauma, but they may be found in any area of the body. Abscesses are formed when the skin is invaded by microorganisms. Cellulitis may precede or occur in conjunction with an abscess. The two most common microorganisms leading to abscess formation are Staphylococcus and Streptococcus.
Treatment of an abscess is primarily through incision and drainage (I&D;). Smaller abscesses (5 mm) may resolve spontaneously with the application of warm compresses and antibiotic therapy. Larger abscesses will require I&D; as a result of an increase in collection of pus, inflammation, and formation of the abscess cavity, which lessens the success of conservative measures.
10. Wound Debridement
Debridement is the removal of dead (necrotic) or infected skin tissue to help a wound heal. It's also done to remove foreign material from tissue. The procedure is essential for wounds that aren't getting better. Usually, these wounds are trapped in the first stage of healing. When bad tissue is removed, the wound can restart the healing process.
11. Lymph node Biopsy
Lymph node biopsy is a test in which a lymph node or a piece of a lymph node is removed for examination under a microscope. The lymphatic system is made up of several lymph nodes connected by lymph vessels. The nodes produce white blood cells that fight infections.
12. Varicose Veins Surgery
Surgery. If endothermal ablation treatments and sclerotherapy are unsuitable for you, you'll usually be offered a surgical procedure called ligation and stripping to remove the affected veins. Varicose vein surgery is usually carried out under general anaesthetic, which means you will be asleep during the procedure.
13. Limb Amputation
Amputation is the removal of a limb by trauma, medical illness, or surgery. As a surgical measure, it is used to control pain or a disease process in the affected limb, such as malignancy or gangrene. In some cases, it is carried out on individuals as a preventive surgery for such problems.
14. Surgery for Hydrocele
A hydrocele is a swelling in the scrotum, the thin sac that holds the testicles. It happens when too much fluid builds up inside. The condition is most common in newborns, though it can happen to anyone with a scrotum.
It may sound or look serious, even painful, but it won’t hurt your baby. It might go away on its own, though you should still see the doctor about it.
15. Circumcision
Circumcision is the removal of the foreskin from the human penis. In the most common procedure, the foreskin is opened, adhesions are removed, and the foreskin is separated from the glans. After that, a circumcision device may be placed, and then the foreskin is cut off
1. Haemorrhoids / Piles Surgery
Haemorrhoids are swollen/enlarged veins in the lowest part of your rectum and anus. Haemorrhoids are one of the most common causes of rectal bleeding. Haemorrhoids can either be internal or external. Internal haemorrhoids develop within the anus or rectum. External haemorrhoids develop outside of the anus.
Symptoms of haemorrhoids include painless bleeding per rectum, pain and itching around the anus, faecal leakage and painful bowel movements. If blood pools in an external haemorrhoid and forms a clot (thrombus), it can result in thrombosed haemorrhoids which causes severe pain where emergency surgical intervention is needed.
Treatment ranges from simple diet modification and laxatives to surgeries depending upon the stage at which patient presentation. Surgery may be open hemorrhoidectomy, which is more traditional or stapler hemorrhoidectomy, which is more popular due to advantages like less pain and discomfort.
2. Fissure in Ano
An anal fissure (fissure-in-ano) is a small tear in the mucosa that lines the opening of the anus. Fissures typically cause severe pain and bleeding with bowel movements. Fissures are quite common in the general population, but are often confused with other causes of pain and bleeding, such as haemorrhoids/piles.
The typical symptoms of an anal fissure include pain and bleeding with bowel movements, most often when you pass hard stools. Patients experience severe pain during, and especially after a bowel movement, lasting from several minutes to a few hours. Patients often notice bright red blood from the anus that can be seen on the toilet paper or on the stool. Between bowel movements, patients with anal fissures are often relatively symptom-free.
Acute fissure may be managed medically whereas chronic fissure may require surgical intervention in the form of controlled division of the part of the internal anal sphincter muscle (sphincterotomy). The success rates reported to be over 90%.
3. Fistula in Ano
An anal fistula is an infected tunnel between the skin and the anus, the muscular opening at the end of the digestive tract. Most anal fistulas are the result of an infection in an anal gland that spreads to the skin. It usually follows an infection that didn’t heal the right way.
Majority of the times fistula is caused by an abscess. It’s rare, but they can also come from conditions like tuberculosis, sexually transmitted diseases, or an ongoing illness that affects your bowels, such as Crohn’s disease or ulcerative colitis.
Symptoms include pain, redness, fever, swelling and discharge of blood or pus from a hole near your anus. Surgery is usually required to treat anal fistula. There are two types of surgeries available. One is a traditional open method, where the muscles around fistula cut and fistula laid open. Other is laser method, which is increasingly popular nowadays because of advantages like no cuts or no stitches, less pain and early return to normal activity.
4. Diabetic foot ulcer
Foot ulcers are most commonly occur as a complication of poorly controlled diabetes, forming as a result of skin tissue breaking down and exposing the layers underneath. They’re most common under your big toes and the balls of your feet, and they can affect your feet down to the bones.
Ulcers form due to a combination of various factors like lack of feeling in the foot, poor circulation, foot deformities, irritation (such as friction or pressure), and trauma. The duration of diabetes also plays an important risk factor. Patients who have diabetes for many years can develop neuropathy, a reduced or complete lack of ability to feel pain in the feet due to nerve damage caused by increased blood glucose levels over time. The nerve damage often can occur without pain, and one may not even be aware of the problem.
All people with diabetes can develop foot ulcers and foot pain at one point in their lifetime, but good foot care can help prevent them. Treatment for diabetic foot ulcers and foot pain varies depending on their causes. It ranges from simple glycemic control to amputation in severe cases. In majority of patients appropriate treatment of a diabetic foot ulcer include prevention of infection, taking the pressure off the area, called “off-loading” footwear, managing blood glucose level and surgical debridement depending on the presentation.
5. Thyroidectomy / Thyroid Surgery
A thyroidectomy is an operation that involves the surgical removal of all or part of the thyroid gland. General, endocrine or head and neck surgeons often perform a thyroidectomy when a patient has thyroid cancer or some other condition of the thyroid gland or goiter.
A thyroidectomy is traditionally a minimally invasive surgery performed through a small horizontal incision in the front of the neck. The entire thyroid gland may be removed or just a single lobe, a portion of a lobe and the isthmus or other structures. Depending on the extent of the operation, patients may need to take the drug levothyroxine, an oral synthetic thyroid hormone.
6. Excision of lumps
Excision of lumps and bumps refers to any minor procedure for skin or subdermal lesions, such as warts, moles, cysts or lipomas. These are typically undertaken under local anaesthesia in a day surgery unit.
7. Pilonidal Sinus and Abscess
A pilonidal sinus (PNS) is a small hole or tunnel in the skin. It may fill with fluid or pus, causing the formation of a cyst or abscess. It occurs in the cleft at the top of the buttocks. A pilonidal cyst usually contains hair, dirt, and debris. It can cause severe pain and can often become infected. If it becomes infected, it may ooze pus and blood and have a foul odor.
A PNS is a condition that mostly affects men and is also common in young adults. It’s also more common in people who sit a lot, like cab drivers.
8. Skin Grafting
Skin grafting is a surgical procedure that involves removing skin from one area of the body and moving it, or transplanting it, to a different area of the body. This surgery may be done if a part of your body has lost its protective covering of skin due to burns, injury, or illness.
A PNS is a condition that mostly affects men and is also common in young adults. It’s also more common in people who sit a lot, like cab drivers.
9. Incision and Drainage for Abscess
An abscess is a confined collection of pus surrounded by inflamed tissue. Most abscesses are found on the extremities, buttocks, breast, axilla, groin, and areas prone to friction or minor trauma, but they may be found in any area of the body. Abscesses are formed when the skin is invaded by microorganisms. Cellulitis may precede or occur in conjunction with an abscess. The two most common microorganisms leading to abscess formation are Staphylococcus and Streptococcus.
Treatment of an abscess is primarily through incision and drainage (I&D;). Smaller abscesses (5 mm) may resolve spontaneously with the application of warm compresses and antibiotic therapy. Larger abscesses will require I&D; as a result of an increase in collection of pus, inflammation, and formation of the abscess cavity, which lessens the success of conservative measures.
10. Wound Debridement
Debridement is the removal of dead (necrotic) or infected skin tissue to help a wound heal. It's also done to remove foreign material from tissue. The procedure is essential for wounds that aren't getting better. Usually, these wounds are trapped in the first stage of healing. When bad tissue is removed, the wound can restart the healing process.
11. Lymph node Biopsy
Lymph node biopsy is a test in which a lymph node or a piece of a lymph node is removed for examination under a microscope. The lymphatic system is made up of several lymph nodes connected by lymph vessels. The nodes produce white blood cells that fight infections.
12. Varicose Veins Surgery
Surgery. If endothermal ablation treatments and sclerotherapy are unsuitable for you, you'll usually be offered a surgical procedure called ligation and stripping to remove the affected veins. Varicose vein surgery is usually carried out under general anaesthetic, which means you will be asleep during the procedure.
13. Limb Amputation
Amputation is the removal of a limb by trauma, medical illness, or surgery. As a surgical measure, it is used to control pain or a disease process in the affected limb, such as malignancy or gangrene. In some cases, it is carried out on individuals as a preventive surgery for such problems.
14. Surgery for Hydrocele
A hydrocele is a swelling in the scrotum, the thin sac that holds the testicles. It happens when too much fluid builds up inside. The condition is most common in newborns, though it can happen to anyone with a scrotum.
It may sound or look serious, even painful, but it won’t hurt your baby. It might go away on its own, though you should still see the doctor about it.
15. Circumcision
Circumcision is the removal of the foreskin from the human penis. In the most common procedure, the foreskin is opened, adhesions are removed, and the foreskin is separated from the glans. After that, a circumcision device may be placed, and then the foreskin is cut off
| Page Contents
- Haemorrhoids / Piles Surgery
- Fissure in Ano
- Fistula in Ano
- Diabetic foot ulcer
- Thyroidectomy / Thyroid Surgery
- Excision of lumps
- Pilonidal Sinus and Abscess
- Skin Grafting
- Incision and Drainage for Abscess
- Wound Debridement
- Lymph node Biopsy
- Varicose Veins Surgery
- Limb Amputation
- Surgery for Hydrocele
- Circumcision
____________________
____________________
____________________
____________________
1. Haemorrhoids / Piles Surgery
Haemorrhoids are swollen/enlarged veins in the lowest part of your rectum and anus. Haemorrhoids are one of the most common causes of rectal bleeding. Haemorrhoids can either be internal or external. Internal haemorrhoids develop within the anus or rectum. External haemorrhoids develop outside of the anus.
Symptoms of haemorrhoids include painless bleeding per rectum, pain and itching around the anus, faecal leakage and painful bowel movements. If blood pools in an external haemorrhoid and forms a clot (thrombus), it can result in thrombosed haemorrhoids which causes severe pain where emergency surgical intervention is needed.
Treatment ranges from simple diet modification and laxatives to surgeries depending upon the stage at which patient presentation. Surgery may be open hemorrhoidectomy, which is more traditional or stapler hemorrhoidectomy, which is more popular due to advantages like less pain and discomfort.
2. Fissure in Ano
An anal fissure (fissure-in-ano) is a small tear in the mucosa that lines the opening of the anus. Fissures typically cause severe pain and bleeding with bowel movements. Fissures are quite common in the general population, but are often confused with other causes of pain and bleeding, such as haemorrhoids/piles.
The typical symptoms of an anal fissure include pain and bleeding with bowel movements, most often when you pass hard stools. Patients experience severe pain during, and especially after a bowel movement, lasting from several minutes to a few hours. Patients often notice bright red blood from the anus that can be seen on the toilet paper or on the stool. Between bowel movements, patients with anal fissures are often relatively symptom-free.
Acute fissure may be managed medically whereas chronic fissure may require surgical intervention in the form of controlled division of the part of the internal anal sphincter muscle (sphincterotomy). The success rates reported to be over 90%.
3. Fistula in Ano
An anal fistula is an infected tunnel between the skin and the anus, the muscular opening at the end of the digestive tract. Most anal fistulas are the result of an infection in an anal gland that spreads to the skin. It usually follows an infection that didn’t heal the right way.
Majority of the times fistula is caused by an abscess. It’s rare, but they can also come from conditions like tuberculosis, sexually transmitted diseases, or an ongoing illness that affects your bowels, such as Crohn’s disease or ulcerative colitis.
Symptoms include pain, redness, fever, swelling and discharge of blood or pus from a hole near your anus. Surgery is usually required to treat anal fistula. There are two types of surgeries available. One is a traditional open method, where the muscles around fistula cut and fistula laid open. Other is laser method, which is increasingly popular nowadays because of advantages like no cuts or no stitches, less pain and early return to normal activity.
4. Diabetic foot ulcer
Foot ulcers are most commonly occur as a complication of poorly controlled diabetes, forming as a result of skin tissue breaking down and exposing the layers underneath. They’re most common under your big toes and the balls of your feet, and they can affect your feet down to the bones.
Ulcers form due to a combination of various factors like lack of feeling in the foot, poor circulation, foot deformities, irritation (such as friction or pressure), and trauma. The duration of diabetes also plays an important risk factor. Patients who have diabetes for many years can develop neuropathy, a reduced or complete lack of ability to feel pain in the feet due to nerve damage caused by increased blood glucose levels over time. The nerve damage often can occur without pain, and one may not even be aware of the problem.
All people with diabetes can develop foot ulcers and foot pain at one point in their lifetime, but good foot care can help prevent them. Treatment for diabetic foot ulcers and foot pain varies depending on their causes. It ranges from simple glycemic control to amputation in severe cases. In majority of patients appropriate treatment of a diabetic foot ulcer include prevention of infection, taking the pressure off the area, called “off-loading” footwear, managing blood glucose level and surgical debridement depending on the presentation.
5. Thyroidectomy / Thyroid Surgery
A thyroidectomy is an operation that involves the surgical removal of all or part of the thyroid gland. General, endocrine or head and neck surgeons often perform a thyroidectomy when a patient has thyroid cancer or some other condition of the thyroid gland or goiter.
A thyroidectomy is traditionally a minimally invasive surgery performed through a small horizontal incision in the front of the neck. The entire thyroid gland may be removed or just a single lobe, a portion of a lobe and the isthmus or other structures. Depending on the extent of the operation, patients may need to take the drug levothyroxine, an oral synthetic thyroid hormone.
6. Excision of lumps
Excision of lumps and bumps refers to any minor procedure for skin or subdermal lesions, such as warts, moles, cysts or lipomas. These are typically undertaken under local anaesthesia in a day surgery unit.
7. Pilonidal Sinus and Abscess
A pilonidal sinus (PNS) is a small hole or tunnel in the skin. It may fill with fluid or pus, causing the formation of a cyst or abscess. It occurs in the cleft at the top of the buttocks. A pilonidal cyst usually contains hair, dirt, and debris. It can cause severe pain and can often become infected. If it becomes infected, it may ooze pus and blood and have a foul odor.
A PNS is a condition that mostly affects men and is also common in young adults. It’s also more common in people who sit a lot, like cab drivers.
8. Skin Grafting
Skin grafting is a surgical procedure that involves removing skin from one area of the body and moving it, or transplanting it, to a different area of the body. This surgery may be done if a part of your body has lost its protective covering of skin due to burns, injury, or illness.
A PNS is a condition that mostly affects men and is also common in young adults. It’s also more common in people who sit a lot, like cab drivers.
9. Incision and Drainage for Abscess
An abscess is a confined collection of pus surrounded by inflamed tissue. Most abscesses are found on the extremities, buttocks, breast, axilla, groin, and areas prone to friction or minor trauma, but they may be found in any area of the body. Abscesses are formed when the skin is invaded by microorganisms. Cellulitis may precede or occur in conjunction with an abscess. The two most common microorganisms leading to abscess formation are Staphylococcus and Streptococcus.
Treatment of an abscess is primarily through incision and drainage (I&D;). Smaller abscesses (5 mm) may resolve spontaneously with the application of warm compresses and antibiotic therapy. Larger abscesses will require I&D; as a result of an increase in collection of pus, inflammation, and formation of the abscess cavity, which lessens the success of conservative measures.
10. Wound Debridement
Debridement is the removal of dead (necrotic) or infected skin tissue to help a wound heal. It's also done to remove foreign material from tissue. The procedure is essential for wounds that aren't getting better. Usually, these wounds are trapped in the first stage of healing. When bad tissue is removed, the wound can restart the healing process.
11. Lymph node Biopsy
Lymph node biopsy is a test in which a lymph node or a piece of a lymph node is removed for examination under a microscope. The lymphatic system is made up of several lymph nodes connected by lymph vessels. The nodes produce white blood cells that fight infections.
12. Varicose Veins Surgery
Surgery. If endothermal ablation treatments and sclerotherapy are unsuitable for you, you'll usually be offered a surgical procedure called ligation and stripping to remove the affected veins. Varicose vein surgery is usually carried out under general anaesthetic, which means you will be asleep during the procedure.
13. Limb Amputation
Amputation is the removal of a limb by trauma, medical illness, or surgery. As a surgical measure, it is used to control pain or a disease process in the affected limb, such as malignancy or gangrene. In some cases, it is carried out on individuals as a preventive surgery for such problems.
14. Surgery for Hydrocele
A hydrocele is a swelling in the scrotum, the thin sac that holds the testicles. It happens when too much fluid builds up inside. The condition is most common in newborns, though it can happen to anyone with a scrotum.
It may sound or look serious, even painful, but it won’t hurt your baby. It might go away on its own, though you should still see the doctor about it.
15. Circumcision
Circumcision is the removal of the foreskin from the human penis. In the most common procedure, the foreskin is opened, adhesions are removed, and the foreskin is separated from the glans. After that, a circumcision device may be placed, and then the foreskin is cut off
| Page Contents
- Haemorrhoids / Piles Surgery
- Fissure in Ano
- Fistula in Ano
- Diabetic foot ulcer
- Thyroidectomy / Thyroid Surgery
- Excision of lumps
- Pilonidal Sinus and Abscess
- Skin Grafting
- Incision and Drainage for Abscess
- Wound Debridement
- Lymph node Biopsy
- Varicose Veins Surgery
- Limb Amputation
- Surgery for Hydrocele
- Circumcision
| Types of Laparoscopic Procedures
____________________
____________________
____________________
____________________